Understanding the Importance of the Advance Beneficiary Notice (ABN) in Medicare
Navigating the complexities of Medicare can be challenging for both healthcare providers and patients. One critical tool in this landscape is the Advance Beneficiary Notice of Non-coverage (ABN), Form CMS-R-131. This form is essential in helping Medicare Fee-for-Service (FFS) patients make informed decisions about their care, particularly when it comes to items and services that Medicare typically covers but might not in specific situations.
Decoding Denials: Track Your Denials and Identify Payer Trends
The world of medical insurance is complex, and having a claim denied is a frustrating setback, potentially leading to financial burdens and increased stress. However, it’s not the end of the road. Let’s look at some common reasons behind denials for medical insurance claims and how to handle them effectively.
Unlocking Success: Key Performance Indicators in Revenue Cycle Management
In the ever-evolving healthcare landscape, revenue cycle management (RCM) is essential to the financial success of medical organizations. Effective RCM ensures accurate and timely reimbursement for services rendered, optimizes cash flow, and enhances overall operational efficiency. Key Performance Indicators (KPIs) are paramount to monitoring and measuring RCM processes’ performance. KPIs act as navigational tools, offering insights into critical aspects of revenue cycle performance. In this blog, we’ll delve into key indicators that can drive success.
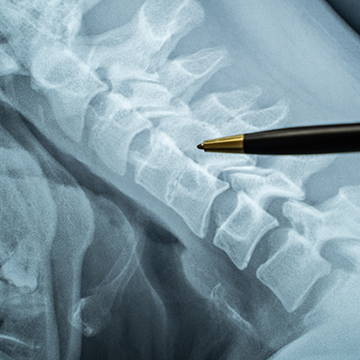
Mastering Documentation for Spinal Cord Stimulators
Spinal cord stimulators are devices implanted into the hip or lower back that contain wires attached to the spinal cord. These wires deliver continuous low-voltage electrical currents, interrupting pain signals to the brain. While this procedure can be an effective treatment for patients, having all the proper documentation is essential.
While not all Medicare Administrative Contractors (MACs) have a local coverage determination (LCD), they all refer back to the national coverage determination (NCD) for their medical reviews.
Potential Changes to Medicare’s Urine Drug Screen Policies
Urine drug screen testing may be deemed medically necessary in several situations, depending on the specific circumstances and a provider’s judgment. Here are some common instances where urine drug screen testing may be considered medically necessary:
- Monitoring medication compliance: Urine drug screens can ensure that patients take prescribed medications as directed, particularly in cases where there is a concern about potential misuse, non-compliance, or diversion of controlled substances.
- Substance abuse assessment: Urine drug screens are frequently used in a comprehensive evaluation to assess substance abuse or addiction. They can help providers identify the presence of illicit drugs or prescription medication misuse, helping develop appropriate treatment plans.
- Medication management in pain management or addiction treatment: For patients receiving treatment for chronic pain or substance abuse disorders, urine drug screens are often used to monitor medication adherence, detect the presence of unauthorized substances, or identify potential drug interactions.
Best Clinical Workflows in Pain Management.
Pain management practices must establish efficient and patient-centric clinical workflows with the increasing prevalence of pain-related conditions. By optimizing these workflows, providers can streamline processes, enhance patient care, and achieve better outcomes. Let’s explore some of the best clinical workflows in pain management practice that can contribute to improved patient experiences and overall treatment success.
New Policy for 2023 Sacroiliac Joint Procedures.
Effective March 19, 2023, Medicare has created a new policy for Sacroiliac Joint Procedures. Several states did not previously have a policy for these procedures, and with the creation of the new policy, not following the items outlined could result in audits and payment recoupments. As a practice, you must ensure you are scheduling and documenting appropriately to capture the necessary information listed in the new policy to prevent takebacks by Medicare. The new rules and regulations outline different areas, such as required post-procedure relief, specific diagnoses allowed, and the exclusion of previously paid procedures that are now not covered. Below are a few of the specifics:
Is your practice up-to-date with payer reimbursement and medical necessity policies?
Staying up-to-date with payer reimbursement and medical necessity policies is essential for your practice. Jessica Armpriester, ConfirmaMD’s Director of Revenue Cycle Integrity, has what you need to know for success. Jessica and her team stay current on new payer policies and actively educate and communicate with providers and staff. She works to break down the communication barrier between payers and physicians.
Reimbursement policies ensure a practice or facility is paid appropriately based on the codes used to describe the services provided. The absence of a policy does not indicate that a service is covered. These are determined based on the individual patient benefit package. Staying up to date with reimbursement helps a practice know what codes are covered and approved by insurance.
When was the last time you negotiated your contract with commercial payers?
When was the last time you negotiated your contract with commercial payers? This edition of N2K emphasizes the importance of payer contracting. Our Director of Contracting & Credentialing, Sandy King, joined the ConfirmaMD team in December 2020 with almost 30 years of relevant healthcare experience, including over 17 years in Managed Care Contracting and Credentialing. She and her team are invaluable in payer contracting, and listed below are the areas they can assist your practice with:
Does “NO AUTHORIZATION REQUIRED” really mean you will be paid?
Prior authorization is when the provider requests a pre-service review to determine coverage and obtain approval from an insurance carrier to pay for a proposed treatment or service. This approval is based on medical necessity, medical appropriateness, and benefit limits at the review time. If the insurance requires prior authorization, you must obtain it before service as the performing or ordering physician. Remember: insurance prior authorization is still not guaranteed payment for a planned procedure. It is just a pre-service review. Prior authorizations are usually only needed for more costly procedures where alternative treatment requirements would have been tried and failed before moving to a more invasive procedure.
Importance of Insurance Verification
Insurance verification should always be high on your practice’s list of priorities. Quality front desk staff adequately trained in insurance verification is worth the investment. The verification process is the first and most significant medical billing and coding step. Due to the always changing and increasingly complex healthcare environment, you will need to pay close attention to validating coverage, benefits, co-payments, and deductibles. The attention required to verification is crucial, and medical care providers must understand the insurance verification process and its importance in the healthcare industry.
Medicare Payment Changes: G Codes
With the new year comes new G codes, and ConfirmaMD’s Billing/Coding Supervisor Joy Baker is here to break them down. Joy and her team work with every ConfirmaMD client account daily to review, bill, or code out their charges. She also provides clients with constant feedback on billing, insurance, or documentation issues. Now she tells us what you need to know about two new codes that became effective on January 1, 2023: G3002 and G3003.
TPE (Targeted Probe and Educate) Audits- What does it mean for you?
The What: Medicare Targeted Prob Audits (TPE) are a hot topic for practices right now.
The Who: CMS is instructing Medicare Administrative Contractors to (MAC) to conduct these TPE Audits.
The Why: WPS, which is jurisdiction 8, stated that over 70% of the practices they have audited failed the first round. Here is a look at where practices are coming up short.
Epidural and Facet Audits –
What does it mean for you?
The What: Epidural Steroid Injections and Facet Joint Interventions Audits
The Who: Most all Providers are affected. After being made aware that several physicians are being audited, our staff is concerned that most practices are having difficulty conforming to the LCDs (Local Coverage Determination) and medical policies.
The Why: To assist you in compliantly documenting these procedures, ConfirmaMD is passing along an algorithm published by ASIPP. You can use this algorithmic approach whenever you see your patients by utilizing these checklists for each patient prior to performing epidural steroid injections and facet joint interventions.
Learn something valuable to your practice?
Stay notified of when we publish new blogs: